University of Wisconsin Center for Cooperatives
Research on the Economic Impact of Cooperatives
Healthcare
Overview
Cooperatives have been part of the U.S. healthcare system since the early 1900s, when hospitals formed the earliest purchasing groups. Although joint purchasing by hospitals is still the most active subsector within healthcare, organizations and individuals cooperate to achieve a wide range of health-related goals. Hospitals and clinics save money by engaging in joint purchasing or service delivery; employer groups jointly negotiate better choices in health insurance rates for their employees; cooperatives/collectives offer controlled access to medical marijuana; worker-owned homecare cooperatives strive to improve service to clients through better working conditions for their workers; and provider networks cooperate to improve rural health care. The organizations may be organized as nonprofits or cooperatives, serving local, regional and/or national markets.
History
The first group purchasing organization in health care was formed in 1910 to purchase laundry services in New York. Currently, >600 group purchasing organizations exist, and most hospitals belong to at least one organization. These organizations negotiate with vendors for a wide range of hospital supplies and services.
In the 1970s and 1980s, rural areas in the U.S. were losing their doctors, hospitals and clinics. Rural health care providers responded by forming health networks. Some early networks were organized as cooperatives, but most are nonprofits with boards that include a large percentage of network members. Networks may offer their members administrative services (such as legal advice, coding assistance, financial consulting, and computer/networking expertise), human resource-related services (such as worker recruitment and professional development), specialized medical services (such as speech or audiology), quality assurance expertise, and joint purchasing.
In the 1970s, in response to rising health insurance costs, employers began to form groups to purchase health insurance. Many purchasing groups were cooperatives. More than 25 states have statutes that promote state- or employer-sponsored purchasing cooperatives. Much of the legislation was in place by the early 1990s, although some legislative activity continues. Many policy makers and communities hoped that the cooperatives would achieve significant cost savings, but analysts recognized the difficulty of avoiding adverse selection without some type of mandated use. Although legislation that would have mandated state or employer-sponsored purchasing cooperatives was discussed during the Clinton health care reform debates, it never passed. Furthermore, while the employer groups are consistently referred to as cooperatives, their business structure varies. For example, in California, an early purchasing cooperative, Health Insurance Plan of California, was originally operated by a state agency. It was later transferred to a nonprofit organization, the Pacific Business Group on Health. In Texas, legislation was passed in 1993, 2003, and 2005 that authorized groups of employers to form cooperatives to purchase health insurance. The cooperatives are required to form as nonprofits and then register as purchasing cooperatives with the Texas Department of Insurance.
After the passage of Proposition 215 in 1996, which legalized medical marijuana in California, dozens of cooperatives, collectives, and buying clubs were established to distribute the drug. Guidelines for the cooperatives/collectives were articulated in California SB420, which passed in 2004 and allowed consumers to grow small quantities of marijuana collectively. To operate legally in California, they must follow guidelines that include operating as nonprofit cooperatives or collectives, paying sales taxes, and allow purchase only by patients or care-givers.
Worker-owned home care cooperatives are emerging as a way to both address high staff turnover and to improve the quality of home care services provided to the elderly and disabled. The first worker-owned home care cooperative, Cooperative Home Care Associates (CCHA), was formed in New York City in 1985, as an alternative to nonprofit and private agencies. CCHA’s goal was to reduce turnover and provide quality home care to clients by improving the workplace and compensation for home care paraprofessionals. Since 1985, a small number of additional worker-owned homecare cooperatives have been formed.
The smallest subsector is consumer-owned health maintenance organizations (HMOs). Few HMOs are genuine cooperatives. Most states require HMOs to incorporate under nonprofit or mutual insurance laws. Wisconsin is one of the few states to allow HMOs to incorporate as cooperatives, but to also have nonprofit and charitable status.
Industry Niche
Health care in the U.S. is provided by a combination of nonprofits, commercial enterprises, and the government. Most health care is paid for through insurance plans, which are funded by employers, privately purchased, or provided by the government. The marketplace for health providers and insurers is local, regional, and national, with significant competition in many communities, especially metropolitan areas.
The only subsector with significant market share is the group purchasing organizations (GPOs). Nine organizations represent 80% of volume purchased through GPOs. These organizations include cooperatives, nonprofit organizations, and for-profit companies. Remarkably, 72% of all hospital purchases are through GPOs, and almost all hospitals use at least one GPO contract, with the average hospital using two to four. Although hospitals formed the first GPOs, clinics and long-term care facilities represent a growing membership.
Employer health care coalitions are another influential subsector, although they have not achieved significant cost savings for their members. There are >90 employee health care coalitions. According to a 2002 study, they have successfully allowed members to provide health care coverage choices to their employees, but their market share is small and they have not achieved significant cost savings (Wicks, 2002).
Organizational Structure
Cooperative health care organizations are organized as cooperatives, nonprofits, and corporations. Regardless of legal structure, they operate for the benefit of their members. Some are organized under statutes that specifically authorize cooperatives to perform a function, such as purchasing health care for small employers, or controlling access to medical marijuana. These statutes vary considerably from state to state, and might not define governance or ownership rights and roles.
Boundary Issues, Data Sources, and Population Discovery
For purposes of this analysis we include health care organizations that are organized to benefit a clearly defined group (employers, health care providers, workers, etc.) and are governed by boards that have significant representation from the membership. Although community health centers do exhibit some of these characteristics, they are not included in the sample.
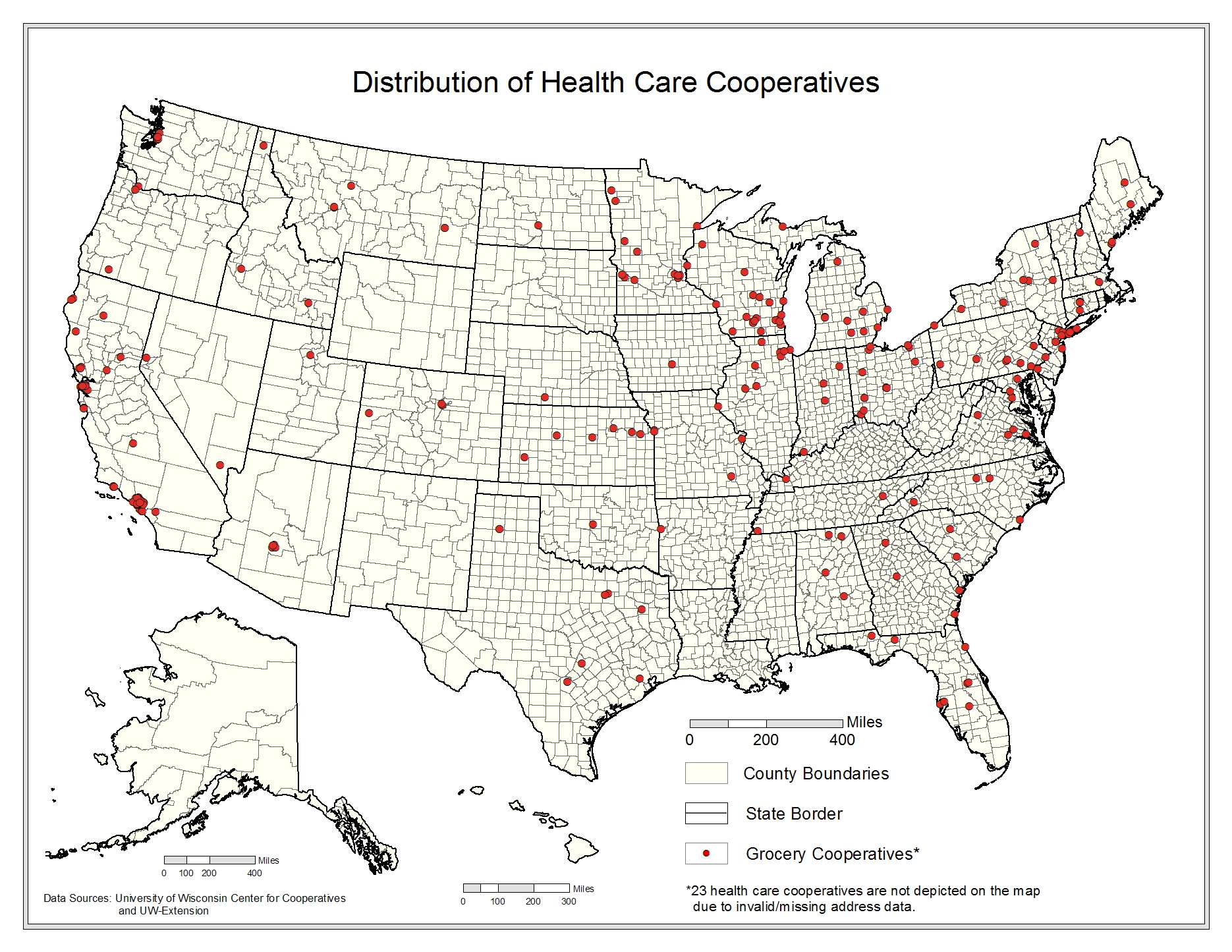
The list for health care cooperatives come from purchasing healthcare cooperatives maintained by National Cooperative Business Association, worker healthcare cooperative lists maintained by Melissa Hoover, USFWC with Prof. Christina Clamp, and primary research. All economic data comes from survey work undertaken by the UWCC. The survey response rate was 58% for healthcare cooperatives, 48% for purchasing healthcare cooperatives, and 32% for worker healthcare cooperatives, and all reporting cooperatives provided 2007 fiscal year-end data. Revenue and employment data for purchasing cooperatives was supplemented from Onesource. The data collection and survey methodology is discussed in detail in the Data Collectionsection in the Appendix
Economic Impacts
Table 4-3 shows that we have data from 192 health-care cooperatives and collectively these firms account for >$1B in assets, >$3B in sales revenue, and pay $283M in wages. There are approximately 961,000 memberships and 73,000 employees. As shown in Table 4-3.1, by extrapolating to the entire population (305 firms) and adding indirect and induced impacts to this activity, health-care cooperatives account for >$5B in revenue, close to 500,000 jobs, $1B in wages paid, and >$1B in valued-added income.
| Economic Impact | Multiplier | Units | Direct | Indirect | Induced | Total | |
|---|---|---|---|---|---|---|---|
| Revenues | 1.011 | million $ | 5,157 | 25 | 30 | 5,211 | |
| Total Income | 1.717 | 727 | 222 | 299 | 1,248 | ||
| Wages | 1.816 | 561 | 206 | 252 | 1,019 | ||
| Employment | 1.535 | jobs | 262,844 | 56,577 | 84,165 | 403,586 | |